1. Respiratory diseases
Around 15 to 20 percent of the German population suffers from acute or chronic respiratory disease. According to the German Federal Statistical Office, lung disease is the third most common cause of death after cardiovascular diseases and cancer. The incidence of respiratory diseases is expected to increase by about 25 percent over the next few years [1].
When we breathe, air travels through our airways to reach the smallest structures of our lungs – tiny air sacs known as alveoli. In the alveoli, the oxygen required by every cell in the body passes into tiny blood vessels called capillaries, while “used” air in the form of carbon dioxide passes from the bloodstream into the lungs to be exhaled. Airway damage caused by bacterial or viral infections or by smoking can interfere with this orderly exchange of gases and weaken the entire body.
The airway can be divided into the upper airway (upper respiratory tract), which includes the nasal cavity, pharynx, and larynx, and the lower airway (lower respiratory tract), which includes the trachea (windpipe) as well as the lungs and lung tissue. Airway damage can lead to upper respiratory tract disease or lower respiratory tract disease, depending on where the damage occurs. Typical upper respiratory tract diseases include colds with a sore throat and runny nose, while lower respiratory tract diseases include conditions such as pneumonia (inflammation of the lung) or bronchial asthma. There are many causes of respiratory disease, with infections, autoimmune disease, and smoking being among the most common.
Acute and chronic respiratory diseases
Besides the location of the damage, the duration of illness is also important when it comes to diagnosis and treatment. While acute respiratory diseases such as the common cold, acute bronchitis, pharyngitis, and tonsillitis are almost always caused by viruses or bacteria and usually clear up within a week or two, the symptoms and airway damage associated with chronic diseases generally last longer than eight to twelve weeks. Chronic respiratory diseases include conditions such as bronchial asthma and chronic obstructive pulmonary disease (COPD).
Respiratory infections
Infections are among the most common causes of acute upper respiratory tract disease and occur most frequently during the fall and winter. Young children may have up to ten respiratory tract infections in a year. Infections are usually triggered by respiratory viruses or, rarely, bacteria. This is also the reason why antibiotics – which only work against bacteria – are often ineffective in treating acute upper respiratory tract infections and at worst can even be harmful. You can help your doctor to make a diagnosis by recording your symptoms in a symptom tracker. However, it is not usually possible to distinguish between viral and bacterial infections based on the symptoms alone.
2. Obstructive vs. restrictive lung disease
Common causes of respiratory diseases
Doctors classify lung disease as either obstructive or restrictive. Obstructive lung diseases cause narrowing of the airways with increased airway resistance, which makes it harder to breathe. Obstructive lung diseases can be triggered acutely, for example, by allergies in people with allergic asthma (triggers include pollen, particulate matter, mold, or certain medicines). Chronic conditions in this category include COPD, which is almost always caused by many years of smoking (cigarettes or e-cigarettes, for example).
Restrictive lung diseases, on the other hand, prevent the lungs from expanding fully, which hampers gas exchange in the alveoli. Mechanical problems, such as a broken rib, or damage to the nerves that coordinate the muscles of respiration can both lead to restrictive lung disease. More often, however, the problems lie in the lung itself. For example, there may be fluid in the lung (pulmonary edema), fluid in the pleural cavity (pleural effusion), or pneumonia. In all these cases, the accumulation of fluid in the tissues interferes with gas exchange in the alveoli.
3. Symptoms that may occur
Depending on the cause, respiratory illnesses present with typical symptoms that can help doctors to identify or narrow down the underlying disease. The most common symptoms of respiratory diseases are cough, dyspnea (breathlessness), chest pain, abnormal breath sounds, and increased mucus production. These symptoms may be accompanied by general symptoms such as fever or fatigue.
Differentiating between symptoms
Cough is the most common symptom of respiratory diseases. It occurs in response to airway irritation and is the body’s reflex attempt to clear the airways of unwanted material such as mucus. Cough can be present in almost any respiratory disease. When it is accompanied by fever, this usually indicates an infection. Dyspnea is the medical term for shortness of breath and describes the sensation of not being able to get enough air. Dyspnea may also be caused by various restrictive and obstructive airway diseases. While chest pain may be a sign of structural damage to the lungs or ribcage, it is also a typical symptom of a heart attack. Noisy breathing can be due to airway narrowing caused by, for example, foreign bodies, swelling, or increased mucus production. Like cough, increased mucus production is a sign of airway irritation and is usually due to infection or an asthmatic reaction. The color and volume of the mucus can also provide clues to the underlying disease.
Infection or allergy
Infections and allergies (hay fever and asthma) are two of the most frequent conditions to affect the respiratory tract. They can be differentiated based on a number of features: Allergic reactions are typically recurrent and seasonal and are triggered by exposure to a specific, usually organic, substance such as pollen or animal hair. Symptoms start suddenly and may be accompanied by itching and swelling of the eyelids. Secretions from the nose and lower airway are usually clear and symptoms resolve quickly in response to antiallergic agents such as antihistamines.
Most infections, on the other hand, tend to occur when the weather is cold. Symptoms develop more gradually and are accompanied by other complaints such as headache or sore throat. The airway secretions are not clear and may be discolored. Respiratory tract infections do not respond to treatment with antihistamines.
4. Common clinical presentations of respiratory disease
So far, we have classified respiratory diseases based on their fundamental characteristics, into acute or chronic diseases that can produce either restrictive or obstructive lung dysfunction. The following section explains three common lung diseases in greater detail.
COPD – chronic obstructive bronchitis
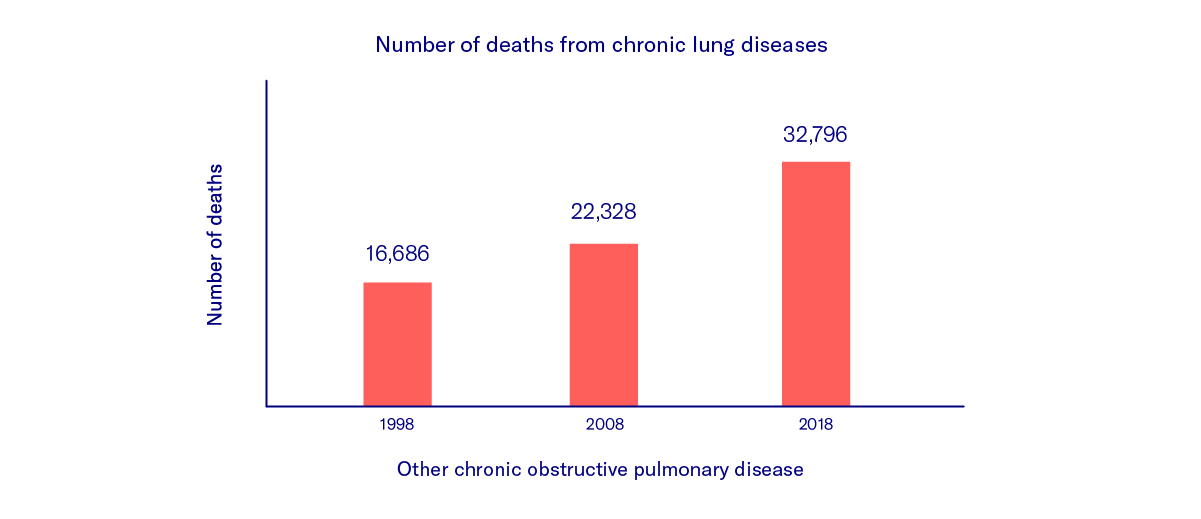
Chronic obstructive pulmonary disease (COPD) is characterized by chronic inflammation of the lungs that leads to pulmonary scarring and irreversible damage. The third most frequent cause of death in the world, COPD is mainly caused by inhaling harmful substances such as cigarette smoke (90% of cases) [1], particulate matter, or exhaust fumes.
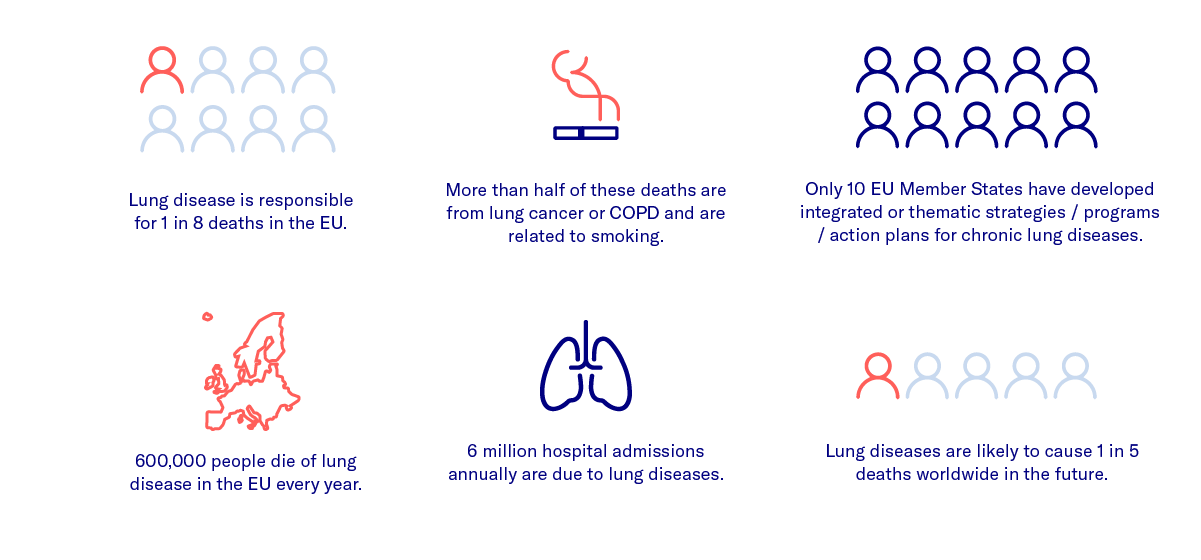
It leads to narrowing of the airways and a reduction in the amount of surface area available for exchanging oxygen and carbon dioxide. Affected patients complain of constant breathlessness and persistent cough. The disease is classified according to the severity, which increases with age and the duration of exposure to harmful substances. Besides medication, the most effective way to slow the progression of the disease is to avoid harmful substances (especially tobacco) [2].
Asthma
Bronchial asthma is a chronic inflammatory airway disease characterized by paroxysmal attacks of chest tightness associated with cough, throat-clearing, and breathlessness. There are several different types of asthma with different causes. It is most commonly caused by allergies to pollen, mold, animal hair, or house dust. Symptoms can be alleviated by taking prescribed antiallergic medications and avoiding substances that trigger attacks. In rare cases, hyposensitization therapy can be used to desensitize patients to trigger substances (allergens). Severe asthma attacks with breathlessness can be life-threatening and require prompt medical attention.
COVID-19
COVID-19 is an acute infectious respiratory disease caused by infection with the coronavirus SARS-CoV-2, which was first detected in Wuhan, China in 2019. The virus can be detected in the saliva and the disease spreads primarily via respiratory (droplet) transmission. The incubation period can last up to two weeks. The risk of transmission is highest just before the onset of symptoms. Flu-like symptoms (especially headache) are common but loss of taste and smell have also been reported. Many affected individuals are either asymptomatic or have very mild symptoms and so can unknowingly spread the virus to others. Active infection can be demonstrated directly in a nose and throat swab while prior infection can be detected by blood tests for antibodies. Around one out of every five affected individuals in Germany requires hospital treatment and fewer than 5% develop lung failure or die from the infection. The risk of having a more serious form of the disease increases with age and pre-existing medical conditions. The average age of patients who have died from the disease is over 80 years [3].
5. Diagnosis
A patient who presents to a doctor with the typical respiratory symptoms described so far will be asked to describe the symptoms in greater detail. The doctor needs to know when the symptoms started, how long they have been present, how frequently they occur, how severe they are, and how they relate to other factors. Pre-existing medical conditions and medications can also provide important clues about the cause of respiratory symptoms.
Clinical examination and investigations
After finding out more about the patient’s symptoms (taking a history), the doctor examines the airways. For more than 200 years, this has involved listening to the patient’s chest using a stethoscope (auscultation). The stethoscope allows the sounds produced by the lungs during inhalation and exhalation to be heard by the human ear. Abnormal breath sounds (doctors often use terms such as wheezing, rhonchi, or rales) and their timing (during inhalation or exhalation) can indicate specific diseases. The doctor also observes how the torso moves during breathing and taps on the patient’s chest (percussion). Technical investigations are not always necessary and are mainly used to diagnose less common disorders. An X-ray or computed tomography (CT) scan provides information on the condition of the lungs and thorax, while spirometry is used to test lung function. During spirometry, the patient is asked to breathe forcefully in and out through the mouth while wearing a nose clip. Important information relating to the lung function can be obtained by analyzing the volume of air breathed in and out as well as the breathing rate. If the results of general investigations suggest the presence of a specific disease, more specialized investigations can be used.
Symptom tracking
Most respiratory diseases have symptoms that can be measured manually, by devices worn on or close to the body (wearables), or even automatically. Many approaches are not concerned with finding a diagnosis, but with documenting existing disease. For example, patients with bronchial asthma can measure their own airflow with a small device (spirometer) to make sure that they are taking the right amount of medication. In this way, patients can play an active role in documenting their symptoms and, if they become more breathless or their airflow decreases, can adjust their medication themselves and show the doctor the record of their symptoms at their next appointment.
Support for faster diagnosis
There are some hurdles to overcome on the way to receiving a proper diagnosis. The more precisely patients can describe their symptoms to the doctor at the initial consultation, the better the chance of receiving an accurate diagnosis. Decision support systems for doctors and symptom trackers for patients can be used to help generate a comprehensive, well-structured medical history. With disease-specific symptom trackers, patients can record relevant symptoms in advance over a prolonged period and show them to the doctor.
The contents of this article reflect the current scientific status at the time of publication and were written to the best of our knowledge. Nevertheless, the article does not replace medical advice and diagnosis. If you have any questions, consult your general practitioner.
Originally published on